Chemobrain Patients: Chemotherapy Side Effects

Chemobrain is defined as a cognitive impairment or cognitive change caused or associated with cancer treatment, either during treatment or in the period after it according to the American Cancer Society.
Patients with chemobrain present as main symptoms: impaired concentration, loss of short-term memory and a feeling of fatigue, making those who suffer from it feel great anguish.
In recent years, there is growing evidence in the medical literature to support an association between the administration of commonly used chemotherapeutic agents and an increased risk of cognitive impairment.
There is a notable complexity between the factors that may be triggering this syndrome, so it could be determined that the etiology of chemobrain is multifactorial and cumulative.
There is still no specific therapy to treat this problem, which unifies several mental constructs, such as attention, memory and executive functions that are affected in patients with chemobrain.
The growing interest in the Spanish Association Against Cancer (AECC) has led to the idea of how to make a therapy that combines several treatments that work separately in people who suffer from cancer or have overcome cancer and try to make a joint proposal.
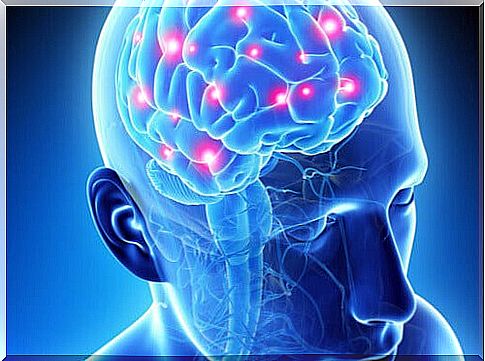
The cognitive functioning of chemobrain patients
In recent years, several studies using neuroimaging techniques have reported structural and functional neuronal changes associated with chemotherapy.
This provides relevant advances to the understanding of the underlying mechanisms of chemotherapy-induced cognitive impairment (Simó, Rifà-Ros, Rodriguez-Fornells & Bruna, 2013).
The theoretical review by Simó, Rifà-Ros, Rodriguez-Fornells and Bruna (2013) on the clinical chemobrain syndrome yields the following data:
- The heterogeneity of MRI studies makes interpretation of the results difficult.
- Structural MRI studies show a diffuse decrease in the volume of gray and white matter.
- Functional magnetic resonance studies show an early decrease in activation in the frontal regions.
- This pattern of deterioration only persists in a subset of patients over time.
- Deterioration found before chemotherapy is probably related to the cancer itself.
Currently, there is no standard approach for the management or prevention of cognitive dysfunction related to chemotherapy treatment. Cross-sectional studies evaluating the cognitive function of patients treated with chemotherapy have other factors that may be contributing to cognitive decline.

Interventions for chemotherapy-associated cognitive impairment
Biofeedback and cognitive behavioral therapy have been used to reduce cognitive dysfunction associated with chemotherapy. In a study that included patients who had stopped chemotherapy at most 5 years before, the biofeedback of the electroencephalogram (EEG) was evaluated to reduce cognitive dysfunction (Álvarez, Meyer, Granoff, & Lundy, 2013).
Patient-reported measures of cognitive function, sleep quality, fatigue, and anxiety / depression were below population norms at baseline and improved within the normal population range after study. 20 neurofeedback training sessions over a 10-week period (Álvarez, Meyer, Granoff, & Lundy, 2013).
In summary, it is reasonable to work with patients to try to modify other factors that can affect cognitive performance. Subjective reports of cognitive dysfunction have been associated with anxiety, depression, fatigue, and sleep disturbances.
Thus, once the clinical picture and its significance are understood, it seems sensible to first address possible confusion problems in patients who have cognitive problems after chemotherapy (Moore, 2014).